EmoniNail™ Science Page
EmoniNail™ exists to help people restore perfect nails and eliminate nail fungus. We use science and data to achieve that purpose. We employ a team of doctors and other experts, covering the areas of medical research literature, product formulation, manufacturing standards, and medical education to ensure we can provide the very best products and resources to our customers. Below you will find the studies which support our treatment method recommendations and product formulas.

Dr. Rohanti Ravikulan
Bachelor of Medicine Bachelor of Surgery (MBBS)
Dr. Rohanti Ravikulan is a qualified medical doctor, freelance medical writer, and medical advisor, who has worked with some of the top organizations in the healthcare industry. She has several scientific publications to her credit and her areas of interests include internal medicine, neurology, and pharmacology. Dr. Ravikulan is passionate about delivering holistic healthcare that is individual-specific rather than disease-specific. During her time in medical school, she designed and developed a patent-pending digital health records system aimed at ensuring treatment transparency among doctors, without compromising patient confidentiality. Dr. Ravikulan strongly believes that quality healthcare is everyone’s birthright and that the complexity of medical information should not stand in the way of one’s own involvement in their healthcare.
The EmoniNail™ Method
The EmoniNail™ Method Works
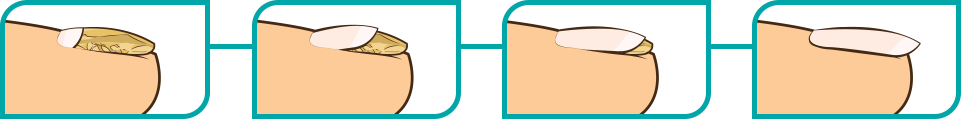
The EmoniNail™ Method Works by helping penetrate the nail plate and delivering powerful anti-fungal agents directly into the nail bed where the fungal infection has taken root.
*Clinical Studies have shown preparing and treating the nail as outlined in The EmoniNail™ Method leads to better, faster, more complete, and more long-lasting results.
EmoniNail™ works by killing fungus on contact and allowing clear beautiful nails to regrow and replace the old infected nails.
* Westerberg D, Voyack M. Onychomycosis: Current Trends in Diagnosis and Treatment. Am Fam Physician. 2013;88(11). https://www.aafp.org/afp/2013/1201/p762.html Accessed November 27, 2019
Key Ingredients

Undecylenic Acid
“The group receiving the undecylenic acid treatment showed significatnt improvement, with fungus eliminated in 88 percent of them after four weeks”
Undecylenic Acid is a US FDA-approved antifungal agent.
Undencylenic acid works by disrupting the growth and multiplication of fungi, including dermatophytes (the most common group of fungi causing fungal nail infections), and yeasts.
In a study of 151 people… the group receiving the undecylenic acid treatment showed significant improvement within just 4 weeks of treatment. ...The fungus was eliminated in 88 percent of the participants after four weeks, compared to only 17 percent of those treated with the placebo powder.
Undecylenic acid belongs to a group of chemical compounds known as “fatty acids” and is found naturally in the body (present in sweat). Commercially, it is obtained from castor oil.
Undecylenic acid works by disrupting the growth and multiplication of fungi, including dermatophytes (the most common group of fungi causing fungal nail infections), and yeasts.
Multiple clinical trials have evaluated the effectiveness of undecylenic acid in fungal infections. In a study of 151 people with fungal infection of the foot, the participants were randomly assigned to receive a topical powder containing 2% undecylenic acid and 20% zinc
undecylenate (the salt form of undecylenic acid) or a placebo powder. The group receiving the undecylenic acid treatment (active powder) showed significant improvement within just 4 weeks of treatment. In 85 of the participants who were assigned to receive the active powder, the fungal infection was caused by dermatophytes, and the fungus was eliminated in 88 percent of them after four weeks, compared to only 17 percent of those treated with the placebo powder.
In another study, 26 diabetic patients with mild, moderate, and severe nail fungal infections went through a new treatment regime. The regime began with a 30-minute warm water soak, followed by filing of the nails, and application of a topical solution containing a cyanoacrylate (a resin) base with 0.1% undecylenic acid and 0.05% hydroquinone. At the end of 3 months, there was a 100% cure rate in patients with mild nail fungal infection (out of 13 patients), 65% cure rate in patients with moderate infection (out of 46 patients), and 35% cure in those with severe nail infection (out of 95 patients).
* McLain N, Ascanio R, Baker C, Strohaver RA, Dolan JW. Undecylenic acid inhibits morphogenesis of Candida albicans. Antimicrob Agents Chemother. 2000;44(10):2873–2875. doi:10.1128/aac.44.10.2873-2875.2000
* Li, X., Jacob, M., Khan, S., Ashfaq, M., Babu, K., Agarwal, A., ElSohly, H., Manly, S. and Clark, A. (2008). Potent In Vitro Antifungal Activities of Naturally Occurring Acetylenic Acids. Antimicrobial Agents and Chemotherapy, 52(7), pp.2442-2448.
* Amsel, L., Cravitz, L., Vanderwyk, R. and Zahry, S. (1979). Comparison of In Vitro Activity of Undecylenic Acid and Tolnaftate against Athlete’s Foot Fungi. Journal of Pharmaceutical Sciences, 68(3), pp.384-385.
* Chretien, J., Esswein, J., Sharpe, L., Kiely, J. and Lyddon, F. (1980). Efficacy of Undecylenic Acid–Zinc Undecylenate Powder in Culture Positive Tinea Pedis. International Journal of Dermatology, 19(1), pp.51-54.

Tea Tree Oil
80% of the participants using the test cream were cured of the fungus, proven by negative fungal tests, while none of the participants in the placebo group achieved cure
Studies have shown that tea tree oil exhibits antifungal properties both in laboratory conditions and in human studies.
After 4 months of treatment, 80% of the participants using the test cream were cured of the fungus, proven by negative fungal tests, while none of the participants in the placebo group achieved cure
Tea tree oil, also known by its botanical name melaleuca oil, is an essential oil obtained from tea trees. Studies have shown that tea tree oil exhibits antifungal properties both in laboratory conditions and in human studies, particularly against some dermatophytes.
In a study of 117 patients with nail fungal infection, the participants were randomized to receive either topical 1% clotrimazole solution (an FDA-approved antifungal agent) or 100% strength tea tree oil for 6 months. At the end of the study, the group receiving topical tea tree oil had cure rates (negative fungal tests in 18% and clinical improvement/resolution in 60% of participants) equal to that of the group receiving the clotrimazole solution (negative fungal tests in 11% and clinical improvement/resolution in 61% of participants).
In another study, 60 people with toenail fungal infection were randomized to receive either a cream containing 2% butenafine hydrochloride (an antifungal agent) and 5% tree tea oil or a placebo cream. After 4 months of treatment, 80% of the participants using the test cream were cured of the fungus, proven by negative fungal tests, while none of the participants in the placebo group achieved cure.11 The rate of cure with this treatment was higher than that seen in another study using butenafine without tea tree oil in the same number of patients.
* Homeyer, D., Sanchez, C., Mende, K., Beckius, M., Murray, C., Wenke, J. and Akers, K. (2015). In Vitro activity of Melaleuca alternifolia (tea tree) oil on filamentous fungi and toxicity to human cells. Medical Mycology, 53(3), pp.285-294.17
* Flores, F., de Lima, J., Ribeiro, R., Alves, S., Rolim, C., Beck, R. and da Silva, C. (2013). Antifungal Activity of Nanocapsule Suspensions Containing Tea Tree Oil on the Growth of Trichophyton rubrum. Mycopathologia, 175(3-4), pp.281-286.
* Inouye S, Uchida K, Yamaguchi H. In-vitro and in-vivo anti-Trichophyton activity of essential oils by vapour contact. Mycoses. 2001;44(3-4):99-107. doi:10.1046/j.1439-0507.2001.00618.x
* Buck D, Nidorf D, Addino J. Comparison of two topical preparations for the treatment of onychomycosis: Melaleuca alternifolia (tea tree) oil and clotrimazole. Journal of Family Practice. 1994;38(6). https://go.gale.com/ps/anonymous?id=GALE%7CA15531820.
* Syed T, Qureshi Z, Ali S, Ahmad S, Ahmad S. Treatment of toenail onychomycosis with 2% butenafine and 5% Melaleuca alternifolia (tea tree) oil in cream. Tropical Medicine and International Health. 1999;4(4):284-287. doi:10.1046/j.1365-3156.1999.00396.x

Sunflower Seed Oil
At the end of the study, 90.5% of the participants that received sunflower oil were cured and the rest of them (9.5%) saw clinical improvement.
Studies have shown that sunflower oil has anti-inflammatory effects as well as the ability to repair damaged skin barrier. Sunflower oil is rich in linoleic acid, a type of fat molecule that is present in and is essential for healthy skin, hair, and nails.
There is also evidence that sunflower oil has antifungal activity in nail infection-causing dermatophytes and yeasts, which has been demonstrated in both laboratory conditions and in humans.
Sunflower oil is obtained from sunflower seeds. Studies have shown that sunflower oil has anti-inflammatory effects as well as the ability to repair damaged skin barrier. Sunflower oil is rich in linoleic acid, a type of fat molecule that is present in and is essential for healthy skin, hair, and nails.
There is also evidence that sunflower oil has antifungal activity in nail infection-causing dermatophytes and yeasts, which has been demonstrated in both laboratory conditions and in humans.14 In one clinical study, 400 patients with nail fungal infection were randomized to receive either topical sunflower oil in ozonized form (where oxygen is added) or 2% ketoconazole cream for 3 months. In the group receiving sunflower oil, improvement was seen within the first month of treatment while the group receiving ketaconazole did not see any results until after the third month. At the end of the study, 90.5% of the participants that received sunflower oil were cured and the rest of them (9.5%) saw clinical improvement. In the ketaconazole group, only 13.5% of patients were cured and 27.5% saw improvement, while the rest had no change. After 3 months, both treatments were stopped and the patients were followed-up after 1 year. In the group that had received sunflower oil, 97.2% remained fungus-free, while only about half of the patients in the ketoconazole group were still fungus-free.
* Lin TK, Zhong L, Santiago JL. Anti-Inflammatory and Skin Barrier Repair Effects of Topical Application of Some Plant Oils. Int J Mol Sci. 2017;19(1):70. Published 2017 Dec 27. doi:10.3390/ijms19010070
* Guerrer LV, Cunha KC, Nogueira MC, Cardoso CC, Soares MM, Almeida MT. "In vitro" antifungal activity of ozonized sunflower oil on yeasts from onychomycosis. Braz J Microbiol. 2012;43(4):1315–1318. doi:10.1590/S1517-838220120004000011
* Gupta A, Paquet M. Improved efficacy in onychomycosis therapy. Clin Dermatol. 2013;31(5):555-563. doi:10.1016/j.clindermatol.2013.06.010
Recent Studies
Emerging Drugs For The Treatment Of Onychomycosis
Aditya K. Gupta & Nadia Stec Expert Opinion on Emerging Drugs, 2019
https://sci-hub.tw/10.1080/14728214.2019.1685493The paper reviews various treatments and their efficacies. The authors conclude that oral treatments are most effective, but have many drug-drug interactions and can hurt the liver. Topical treatments, though preferred, are less effective because of the nail barrier which is practically impenetrable. Overall, treatment options are short term oral therapies (~3 months) or long term topical treatments (>1 year) with patient compliance. Recurrence of infection can be prevented through prophylaxis, disinfection of socks and shoes, and wearing footwear in public places.
Prognostic Factors Influencing The Treatment Outcome Of Onychomycosis Candida
Sandra Widaty, Eliza Miranda, Kusmarinah Bramono, Sri Linuwih Menaldi, Melani Marissa, Caroline Oktarina, Danny Surya, Hening Tirta Kusumawardhani Mycoses, 2019
sci-hub.tw/10.1111/myc.13018The authors looked into what affects the outcome of nail fungal infection caused by Candida. The factors that make the cure harder are: old age, presence of other conditions (e.g. diabetes, immunocompromised states), multiple sites of infection, duration of infection (the longer the worse the prognosis), and the higher the number of infected nails.
The Dermatologist’s Approach to Onychomycosis
Jenna N. Queller and Neal Bhatia Journal of Fungi, 2015
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5753109/Newer topical agents are more effective than previous agents. The new topical agents approved in the US are solutions with increased nail penetration characteristics and low surface tension. These agents penetrate the nail and through the space between the nail plate and the nail bed. Agents explored in this article are: efinaconazole 10% topical solution (referencing studies with 50% cure rate and efficacy was not dependent upon daily debridement) and tavaborole (cure rate of about 35% and penetration through nail plate approximately 250 times greater than ciclopirox).
Onychomycosis: Treatment And Prevention Of Recurrence
Shari R. Lipner and Richard K. Scher Journal of the American Academy of Dermatology 2018
https://sci-hub.tw/10.1111/myc.13016This is a treatment guidelines update by the American Academy of Dermatology. According to this paper, the first line treatment is still oral antifungal agents, with terbinafine and itraconazole recognized as FDA-approved therapies, and fluconazole and terbinafine pulse-dosing recognized s off-label therapies. Topical agents recognized as FDA-approved are ciclopirox 8%, efinaconazole 10% and tavaborole 5%. The treatment algorithm for systemic and topical agents are as follows: For proximal infection and distal infection affecting >50% of nail area or more than 3-4 nails affected, systemic agents alone are recommended. For superficial infection and distal infection affecting >50% of nail area with up to 3-4 nails infected, a combination of systemic and topical agents are recommended, and for cases where systemic therapy is contraindicated, topical agents alone are recommended.
Oral Antifungal Medication For Toenail Onychomycosis
Sanne Kreijkamp‐Kaspers, Kate Hawke, Linda Guo, George Kerin, Sally EM Bell‐Syer, Parker Magin, Sophie V Bell‐Syer, Mieke L van Driel Cochrane Database of Systematic Reviews, 2017
https://www.cochranelibrary.com/cdsr/doi/10.1002/ 14651858.CD010031.pub2/fullThis is a systematic review article where the data from multiple studies is combined into one. The authors combined 48 studies involving 10,200 participants. The study concluded that terbinafine and azoles were the most effective at eliminating nail fungal infection and better than griseofulvin. Only some studies reported the side effects, but among those that did, terbinafine and azoles had fewer side effects than griseofulvin. The terbinafine and azoles lowere recurrence rates equally, but the evidence on recurrence rates is scarce.
Improving Cure Rates in Onychomycosis
Aditya K. Gupta, Maria Cernea, and Kelly A. Foley Journal of Cutaneous Medicine and Surgery, 2016
https://sci-hub.tw/10.1177/1203475416653734This is a good review article that looks into different treatment strategies. Hard to summarize everything here but in essence the authors explore treatment regimens according to the fungal life cycle, and the benefit of systemic + topical combination therapy against monotherapy. In conclusions, the authors recommend tailoring the treatment to the individual based on their co-existing conditions, using combination therapy, improving nail penetration to topical therapies via different techniques, and using propylactic antifungal therapy to prevent recurrence.
Onychomycosis in the 21st Century: An Update on Diagnosis, Epidemiology, and Treatment
Aditya K. Gupta, Sarah G. Versteeg, and Neil H. Shear Journal of Cutaneous Medicine and Surgery, 2017
https://sci-hub.tw/10.1177/1203475417716362Great review article that looks at the current strategies for diagnosis and management of nail fungal infection. The article has a really important table showing the current approved therapies and their cure rates. According to this table, terbinafine and itraconozole have the highest fungal smear cure and complete cure rates, followed by eficonazole in the topical treatment section. Tavaborole and ciclopirox have lower cure rates and are similar to each other. Laser therapy is reported to be the least effective. The conclusions are in line with the findings reported in this table.
British Association Of Dermatologists' Guidelines For The Management Of Onychomycosis 2014
M. Ameen, J.T. Lear, V. Mada,n M.F. Mohd Mustapa, M. Richardson British Journal of Dermatology, 2014
https://onlinelibrary.wiley.com/doi/full/10.1111/bjd.13358This is the British Associarion of Dermatologists' guidelines for nail fungus treatment. Unlike the American guidelines, monotherapy with topical agents is receommended in superficial white nail infection and early stages of distal under-the-nail infection when >80% of the area is affected. The paper recognizes amorolfine, ciclopirox, and tioconazole, and efinaconazole as topical therapies, but all at a recommendation strength D (insufficient evidence). Terbinafine and itraconazole were recommended at strength A and as first line.
Therapies for Onychomycosis
Aditya K. Gupta, Deanne Daigle, and Maryse Paquet Journal of the American Podiatric Medical Association, 2015
https://sci-hub.tw/10.7547/13-110.1This is a meta-analysis study, which means it combines the data from multiple studies to reach a statistical conclusion. The results showed that terbinafine and itraconazole were the most efficacious, while topical treatments were comparable to fluconazole (the oral treatment). The paper has charted out an algorithm which mainly recommends the use of oral antifungals where possible, and topical agents where oral agents are contraindicated. Eficonazole is the only recognized topical treatment in this paper.
Management of Onychomycosis in Canada in 2014
Aditya K. Gupta and Maryse Paquet Journal of Cutaneous Medicine and Surgery, 2014
https://www.mdedge.com/dermatology/article/99462/ hair-nails/onychomycosis-treatment-united-statesThis is a Canadian Dermatology Association practice guideline paper. There is a treatment algortithm based on the infective pathogen, infected area %, and concomitant medications. In most cases, the paper recommends oral + topical combination therapy, placing higher importance on oral therapy where possible. There is a table of cure rates according to aaffected nail area % for each agent where oral agents, terbinafine and itraconazole have the highest rates for >50% involvement and eficonazole having the highest rate of cure in infections with <65% involvement.
Onychomycosis Treatment in the United States
Arash Taheri, Scott A. Davis, Karen E. Huang, Steven R. Feldman Cutis, 2015
https://www.mdedge.com/dermatology/article/99462/ hair-nails/onychomycosis-treatment-united-statesThis is a study looking at the prevalence of nail fungus and prescribing practices between 1993 and 2010. The key findings from this study were that nail fungal infection is most commonly found in patients older than 35 years, and terbinafine has been the most commonly prescribed antifungal agent, followed by systemic fluconazole, systemic itraconazole, and topical ciclopirox. There are a few other statistics in the study about the most common concomitant infections and number of doctor visits each year.
Tavaborole – A Treatment for Onychomycosis of the Toenails
Aditya K. Gupta & Sarah G. Versteeg Expert Review of Clinical Pharmacology, 2016
https://sci-hub.tw/10.1080/17512433.2016.1206467This is a review article of Tavabarole that explores the mechanism of action, nail penetration, and treatment evidence of 5% tavaborole (topical). The main points include its unique mechanism of action (disrupting the fungal RNA enzyme which stops fungal protein production), its greater nail penetration in comparison to ciclopirox, and its overall safety profile.
Novel Investigational Therapies For Onychomycosis: An Update
Aditya K Gupta & Catherine Studholme Expert Opinion on Investigational Drugs, 2016
https://sci-hub.tw/10.1517/13543784.2016.1142529This review article is about the new drugs currently undergoing testing/investigation for the treatment of nail fungus. A new drug under testing is VT-1161, an oral antifungal that is thought to interact less with the human liver enzymes (thought to contribute to side effects). Initial animal studies showed equal efficacy to terbinafine and superiority to itraconazole with no side effects. Initial human studies with this drug showed that the drug attained higher concentrations in the skin and nail tissue than in the bloodstream suggesting that it could be skin-specific. More trials results are awaited. The study goes on to review data on eficonazole and tavaborole. The study also reviews amorolfine (topical) in a UV-curable gel and the use of amorolfine with CO2 laser therapy, both of which improved the nail penetration of amorolfine and consequently improved efficacy. ME1111 is another novel topical agent that is currently undergoing testing. Its antifungal activity appears to be equal to ciclopirox and higher than that of amorolfine in in vitro studies. Initial animal studies have shown good nail penetration and further studies are awaited.
Clinical Trials Of Lasers For Toenail Onychomycosis: The Implications Of New Regulatory Guidance
Aditya K. Gupta, Kelly A. Foley & Deanne Daigle Journal of Dermatological Treatment, 2017
https://sci-hub.tw/10.1080/09546634.2016.1214670The study reviews the findings from clinical trials that evaluated the efficacy of lasers in nail fungus treatment. The authors concluded that there is insufficient evidence to determine the efficacy of lasers in nail fungus treatment and that the existing evidence is not very favourable. Furthermore, the authors recommend that guidelines be laid down for studies involving lasers so that they are more comparable.
Global Perspectives For The Management Of Onychomycosis
Aditya K. Gupta et al. International Journal of Dermatology, 2018
https://sci-hub.tw/10.1111/ijd.14346This is a review article on nail fungus epidemiology, diagnosis, and treatment practices around the world. In the treatment section there is a great table that displays all the medications approved for the treatment of nail fungus in all the different countries, and there is another table that clearly lays out the warnings, side effects, contraindications, an drug-drug interactions for each oral antifungal agent. Good overview of treatment around the world.
Onychomycosis: Evaluation, Treatment Options, Managing Recurrence, and Patient Outcomes
Aditya K. Gupta et al. International Journal of Dermatology, 2018
https://sci-hub.tw/10.1111/ijd.14346This is a review article that looks into the diagnostic and therapeutic options of nail fungus. It also reports the findings from two new trials on topical agent efinaconazole and tavabarole (with the former shown to be more efficacious). It's a good paper to get an overall idea of treatment strategies, progostic factors, and management of recurrence.
Potential of Ravuconazole and its Prodrugs as the New Oral Therapeutics for Onychomycosis
Hideyo Yamaguchi Medical Mycology Journal, 2016
https://www.jstage.jst.go.jp/article/mmj/57/4/ 57_16-00006/_pdf/-char/jaThis is a review article on a new oral antifungal agent that is currently being studied for nail fungus treatment. The original drug development was stopped, but a prodrug version is currently being studied which Is thought to be efficacious, based on in vitro studies against itraconazole and some preliminary human studies. The phase II trial of the prodrug form is complete and the authors suggest that it could be a better oral medication given its prolonged half-life, which menas that it would need to be less frequently administered and possibly has less side effects. Further data is expected.
Potential of Ravuconazole and its Prodrugs as the New Oral Therapeutics for Onychomycosis
Hideyo Yamaguchi Medical Mycology Journal, 2016
https://www.jstage.jst.go.jp/article/mmj/57/4/ 57_16-00006/_pdf/-char/jaThis is a review article on a new oral antifungal agent that is currently being studied for nail fungus treatment. The original drug development was stopped, but a prodrug version is currently being studied which Is thought to be efficacious, based on in vitro studies against itraconazole and some preliminary human studies. The phase II trial of the prodrug form is complete and the authors suggest that it could be a better oral medication given its prolonged half-life, which menas that it would need to be less frequently administered and possibly has less side effects. Further data is expected.
Terbinafine for Onychomycosis
Matthew K. Hawks, Jedda P. Rupert, And Jennifer E. Svarverud American Family Physician, 2019
https://www.aafp.org/afp/2018/0801/od1.htmlThis article is a short opinion/ review of the most recent evidence on Terbinafine, and references the Cochrane Database meta-analysis study. The overall rating given as part of the article reflects that the benefits of the drug are unclear. There is hardly any new information contributed in this article.
Pharmacotherapy For Onychomycosis: New And Emerging Treatments
Shari R. Lipner Expert Opinion on Pharmacotherapy, 2019
https://sci-hub.tw/10.1080/14656566.2019.1571039This article reviews the currently approved treatments (oral and topical) for nail fungus treatment. There are great tables in the article for each oral and topical treatment that specifies the indication, dosing, contraindications, and warnings for each agent. In the new therapies section, the oral therapies mentioned are fosravuconazole L-lysine ethanolate (F-RVCZ), posaconazole, and VT-1161. The emerging topical treatments mentioned are luliconazole and ME1111.
Update On Current Approaches To Diagnosis And Treatment Of Onychomycosis
Aditya K. Gupta, Rachel R. Mays, Sarah G. Versteeg, Neil H. Shear & Vincent Piguet Expert Review of Anti-infective Therapy, 2018
https://sci-hub.tw/10.1080/14787210.2018.1544891This article focuses on the diagnostic and therapeutic approaches to nail fungus infection. As with other articles, there is mention of the high cure rate of oral agents over topical agents and the importance of combination therapy. However, the key point mentioned in this article is that the emerging topical agents are in solution form instead of lacquer form, which means that they do not have to be removed weekly, which may make patient compliance better. In addition, the authors recommend prophylactic treatment with topical agents to prevent recurrence.
Photodynamic Therapy For Onychomycosis: A Systematic Review
Anil Kumar Bhatta, Uma Keyal, Xiu Li Wang Photodiagnosis and Photodynamic Therapy, 2016
https://sci-hub.tw/10.1016/j.pdpdt.2016.07.010This is a systematic review where the data from multiple studies is combined. There are various types of photodynamic therapies explored, with different types of light. The authors conclude that the evidence is insufficient however some studies have shown exciting results and it is worth exploring this therapeutic approach to nail fungus treatment as it allows better penetration of the nail with much fewer side effects.
Treatment Of Onychomycosis Using A 1064-nm Diode Laser With Or Without Topical Antifungal Therapy: A Single-Center, Retrospective Analysis In 56 Patients
G. C. Weber, P. Firouzi, A. M. Baran, E. Bölke, H. Schrumpf, B. A. Buhren, B. Homey and P. A. Gerber European Journal of Medical Research, 2018
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6199788/This study retrospectively looked at patients with nail fungus who were treated with laser therapy and compared those who concomitantly received topical antifungal treatment and those who didn’t. The study population was only 56 adults, with 29 receiving both laser and antifungals. The results showed that the laser improved treatment effect and that combining it with antifungals had a synergistic effect, with these patients showing improvement quicker.
Topical Therapy For Toenail Onychomycosis: An Evidence-based Review
Aditya K. Gupta, Deanne Daigle, Kelly A. Foley American Joural of Clinical Dertmatology, 2014
https://sci-hub.tw/10.1007/s40257-014-0096-2This is a review article focusing on topical therapies for nail funus treatment. The authors review 28 studies on amorolfine, ciclopirox, tavaborole, and efinaconazole, with findings indicating the efinaconazole came out on top. The authors conclude that topical treatment with amorolfine, ciclopirox, tavaborole, or efinaconazole is appropriate for cases of mild to moderate toenail onychomycosis due to dermatophyte or mixed dermatophyte/Candida infection
Chemical And Physical Strategies In Onychomycosis Topical Treatment: A Review
Tamara Angelo, Lívia Neves Borgheti-Cardoso, Guilherme Martins Gelfuso, Stephânia Fleury Taveira, Tais Gratieri Medical Mycology, 2017
https://academic.oup.com/mmy/article/55/5/461/2628990This article looks at the various techniques that are used to improve the penetration and efficacy of topical treatments. Physical techniques discussed include nail debridement, lasers, and micoporation while chemical techniques include using different vehicles and keratolytic agents. The article goes on to discuss the efficacy of each technique specific to each topical agent.
View Less

View More

Downloadble Content

About Fungal Nail Infection
Fungal Nail Infection, known as onychomycosis or tinea unguium in medical terms, is the most common nail disorder, affecting roughly 1 in 10 people in the general population. This number increases with age, with 1 in 2 adults over 70 years being affected by the disease.

How Emoninail™ Method Works
The EmoniNail™ MethodWorks by penetrating the nail plate and delivering powerful anti-fungal agents directly into the nail bed where the fungal infection has taken root.
Restore Clear Nails with EmoniNail™
-
 Kills Nail Fungus
Kills Nail Fungus -
 Applies Easily with Topical Brush
Applies Easily with Topical Brush -
 Helps Clear Yellow Keratin
Helps Clear Yellow Keratin -
 Natural, Safe and Effective
Natural, Safe and Effective
-
 Unlimited Access to Treatment Support Experts
Unlimited Access to Treatment Support Experts
-
 Guaranteed to Work within 60 Days or Your Money Back
Guaranteed to Work within 60 Days or Your Money Back
-
 It Works
It Works

















